How to Maintain Sterilisation Standards in Dental Practices?
Sterilisation sits at the heart of safe dentistry. Every dental procedure relies on clean, properly processed instruments to protect patients, clinicians, and support staff. When sterilisation standards slip, the consequences can be serious. Patients face higher infection risks, while staff exposure to contaminated instruments can lead to illness, injury, or regulatory action. In dental practices, maintaining consistent sterilisation requires more than basic cleaning. Dental clinics also operate under strict infection control expectations, which place responsibility on practices that support compliance with dental sterilisation standards in Australia.
This blog serves as a practical dental practice sterilisation guide. It explains core principles, outlines clear procedures, and highlights best practices. You will get to know how to identify weak points in current workflows and strengthen them with simple, effective measures.
Understanding Sterilisation in Dental Practices
Sterilisation refers to the complete elimination of all microorganisms, including bacteria, viruses, fungi, and spores. It differs from disinfection, which reduces microbial load without guaranteeing complete elimination. In dentistry, sterilisation is required for instruments that penetrate soft tissue or bone, while disinfection is used for surfaces and non-critical items.
Australian dental practices follow infection control guidance aligned with national health standards and professional bodies. These guidelines outline how dental sterilisation procedures should be performed, monitored, and documented. Compliance supports patient safety while also protecting practices during audits or complaints. A clear understanding of terminology helps teams apply the correct process to each item. Misclassifying instruments can result in underprocessing, which increases infection risk.
Difference Between Sterilisation, Disinfection, And Sanitisation
Sterilisation destroys all microorganisms on instruments such as forceps, scalers, or surgical tools. Steam autoclaving is the most common method.
Disinfection lowers microbial numbers on non-critical surfaces like dental chairs, light handles, and benches. Approved chemical disinfectants are used for this purpose.
Sanitisation focuses on general cleanliness, often applied to floors or waiting areas. It does not replace sterilisation or disinfection in clinical zones.
Why Sterilisation Standards Are Vital
Strong sterilisation protocols protect patients against cross-contamination. They also reduce occupational exposure for dental staff. Regulatory compliance relies on documented processes that demonstrate due diligence. A consistent approach strengthens practice reputation while building patient trust.
Key Steps to Maintain Sterilisation Standards
Effective sterilisation follows a structured workflow. Each stage plays a role in guaranteeing that instruments are safe for reuse.
Instrument Cleaning and Pre-Sterilisation Procedures
All instruments should be treated as contaminated after use. Staff must wear appropriate PPE during handling. Pre-cleaning removes visible debris, blood, or tissue that can compromise the effectiveness of sterilisation. Manual cleaning uses long-handled brushes with detergent, followed by thorough rinsing. Ultrasonic cleaners provide deeper cleaning by loosening debris through vibration.
Instruments should then be dried completely. Moisture left behind can interfere with packaging integrity or sterilisation cycles. Inspection is essential at this stage. Check for damage, corrosion, or retained debris. Damaged items should be removed from circulation.
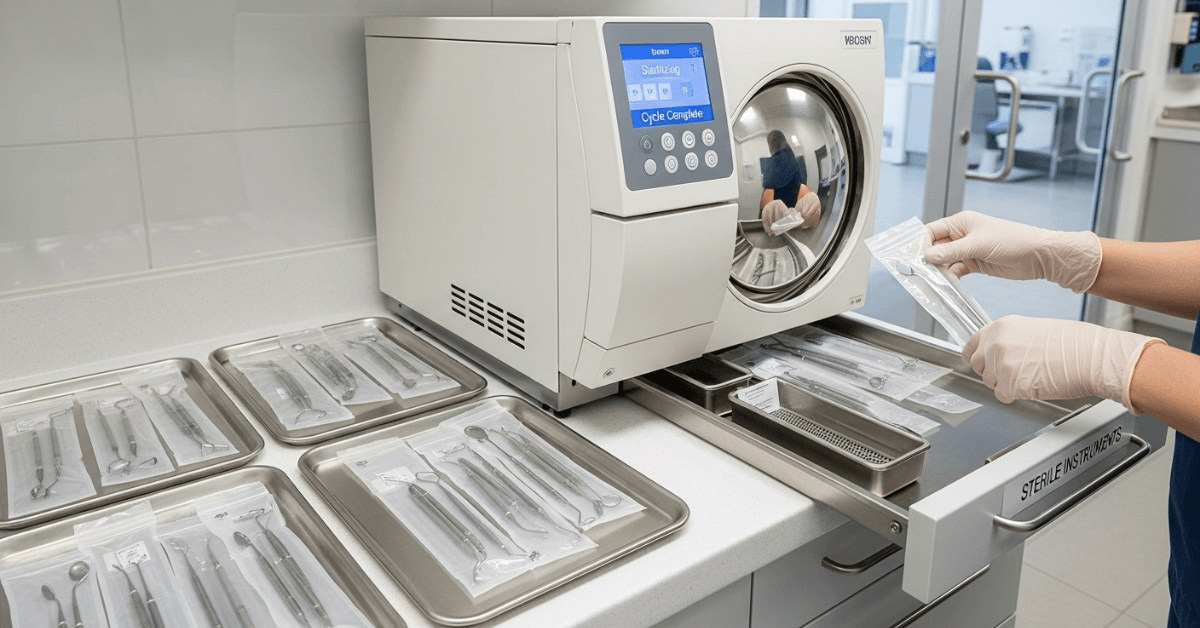
Sterilisation Methods and Equipment
Steam autoclaves remain the preferred option for heat-stable dental instruments. Correct loading guarantees steam contact with all surfaces. Overloading can reduce effectiveness. Follow manufacturer instructions for temperature, pressure, and cycle duration.
Dry heat sterilisation may be used for specific items, though cycle times are longer. Chemical vapour systems require controlled conditions and correct ventilation. Heat-sensitive items should only undergo approved chemical sterilisation when indicated. Regular maintenance of sterilisation equipment is critical. Faulty units compromise outcomes even with correct technique.
Packaging and Storage of Sterilised Instruments
Packaging protects instruments after sterilisation. Use approved wraps or pouches that allow steam penetration. Include chemical indicators inside each pack. Label packs with date, contents, and steriliser number if applicable.
Store sterilised items in clean, dry cupboards away from high-traffic areas. Avoid crushing or bending packaging. Compromised packs must be reprocessed.
Surface and Environmental Disinfection
Clinical surfaces require cleaning between patients. Focus on chairs, trays, switches, and handles. Remove visible soil before applying disinfectant. Follow manufacturer instructions for dilution and contact time.
Barrier protection reduces surface contamination and speeds turnaround. Dental unit waterlines also need routine maintenance to prevent microbial growth.
Monitoring and Validating Sterilisation
Monitoring verifies that sterilisation processes work as intended. It also provides evidence during audits.
Different Indicators
There are biological, mechanical, and chemical indicators. Mechanical indicators include time, temperature, and pressure readings from autoclave displays or printouts. Review these after every cycle. Chemical indicators change colour when exposure parameters are met. They confirm pack-level conditions.
Biological indicators use spores to test the steriliser's effectiveness. Conduct these tests on a scheduled basis, usually weekly. Failed tests require immediate investigation and corrective action.
Record-Keeping and Documentation
Maintain logs for each sterilisation cycle. In which you will include the operator name, cycle details, results, and corrective steps if issues arise. Documentation supports traceability and demonstrates compliance with dental sterilisation protocols for dental practices.
Staff Training and Compliance
Sterilisation standards depend on staff competence and consistency.
Regular Training Programs
Training should cover infection control principles, equipment use, and updated guidelines. New staff require induction training, while existing staff benefit from refresher sessions. Training records should be kept current.
Personal Protective Equipment (PPE) Usage
PPE protects staff during instrument processing. Gloves, masks, eyewear, and gowns must be worn correctly. Proper removal reduces contamination risk. Replace disposable items after each task.
Auditing and Accountability
Internal audits help identify gaps before they become problems. Use checklists to assess compliance with procedures. Address issues promptly through retraining or workflow adjustment.
Common Mistakes and How to Avoid Them
- Skipping pre-cleaning steps reduces sterilisation effectiveness. Organic debris shields microorganisms from heat or chemicals.
- Overloading autoclaves prevents proper steam circulation. Follow the loading diagrams provided by manufacturers.
- Ignoring expiry dates on sterilised packs increases contamination risk. Rotate stock and inspect packaging regularly.
- Human error remains a common cause of failure. Clear protocols, visual reminders, and accountability systems reduce mistakes.
New Technologies and Best Practices
Modern sterilisation workflows benefit from automation and digital tracking. Barcode systems link instruments to cycles, which improves traceability. Single-use items reduce reprocessing demands for certain procedures.
Staying informed about guideline updates supports continuous improvement. Practices that review procedures regularly adapt more effectively to regulatory changes and emerging risks.
Final Thoughts
Maintaining high sterilisation standards protects patients, staff, and practice reputation. Clear understanding of sterilisation in dental practices, structured workflows, regular monitoring, and staff training all contribute to safer care. Consistency remains the key factor. By following documented procedures for sterilisation and auditing performance, practices meet regulatory expectations while reducing infection risk. Ongoing review guarantees systems remain effective as technology and guidance evolve.
You can buy dental tools online from Dentify Dental with confidence, knowing that each product meets Australian regulatory compliance standards.
Disclaimer
The content provided here on the sterilization, cleaning, and reprocessing of surgical and medical instruments is strictly for informational and educational purposes only. This information is not a substitute for professional training, certification, or the manufacturer's official Instructions for Use (IFU). Sterilization is a critical, complex process that demands strict adherence to regulatory standards; improper technique can cause serious harm, including patient infection. All healthcare personnel must follow their facility's established protocols and the specific IFU for every instrument and piece of equipment. By using this blog, you agree that the author/owner holds no liability for any damages or consequences resulting from the application or misuse of this information.










