How Are Surgical Instruments Cleaned and Disinfected?
Maintaining sterile surgical instruments is vital for patient safety and infection prevention. Every tool used in a medical or dental procedure must go through a precise cleaning and disinfection process to remove contaminants such as blood, tissue, and microorganisms. This process not only safeguards patients but also extends the lifespan and performance of the instruments.
Understanding the Importance of Instrument Sterilisation
Surgical instruments come into direct contact with internal tissues, making sterilisation critical to prevent infections and cross-contamination. Even minor lapses in cleaning or sterilisation can introduce harmful bacteria or viruses into the surgical field, compromising patient safety.
A structured approach to cleaning and disinfection of surgical instruments involves multiple steps, each designed to progressively eliminate contaminants before the instruments are used again.
Properly cleaned and sterilised tools not only protect patients but also improve surgical outcomes and maintain the integrity of the healthcare facility’s reputation.
Steps for Cleaning and Disinfecting Surgical Instruments
Step One: Pre-Cleaning and Initial Rinse
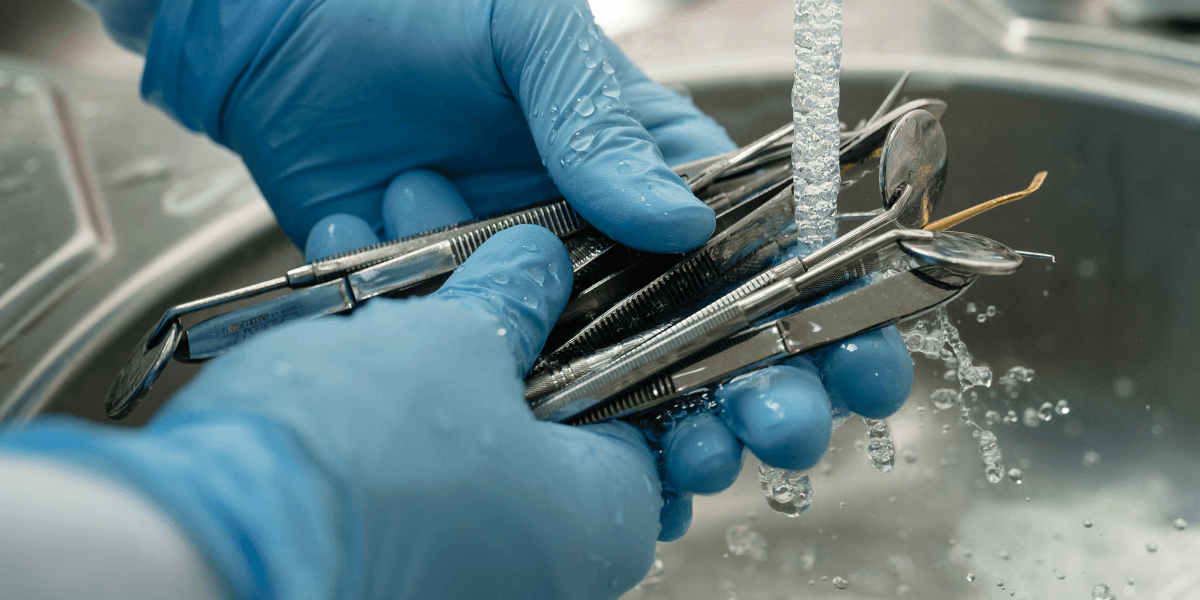
The first stage begins immediately after an operation. Instruments are typically rinsed under cold running water to remove visible debris such as blood, tissue fragments, and other organic matter. Using hot water at this stage is discouraged, as it can cause proteins to coagulate, making residues harder to remove.
Pre-cleaning is usually done near the operating area to prevent drying of contaminants on the instrument’s surface. The goal is to reduce the microbial load before instruments are transferred to the central sterilisation department.
Step Two: Manual Cleaning
Manual cleaning of surgical instruments is performed when instruments require delicate handling or contain intricate parts that automated systems might miss. Trained staff use brushes, detergent solutions, and enzymatic cleaners to dissolve and remove organic residues. Key steps in manual cleaning include:
- Using soft-bristled brushes to reach crevices and joints.
- Rinsing instruments thoroughly after scrubbing.
- Maintaining a neutral pH cleaning solution to prevent corrosion.
- Wearing protective gloves and face shields to maintain safety during handling.
This phase requires close attention since any residue left behind can interfere with later sterilisation stages.
Step Three: Ultrasonic Cleaning
After manual washing, most facilities use ultrasonic cleaning machines for deeper decontamination. These devices work on the principle of cavitation; high-frequency sound waves create microscopic bubbles that collapse and dislodge hidden contaminants from the surface of the instruments.
Ultrasonic cleaning is highly effective for complex or hinged tools such as forceps, clamps, and dental pliers. The solution inside the machine often contains specialised detergents that break down proteins and fats without damaging metal surfaces.
This step is vital before proceeding to the disinfection of surgical instruments, as it makes sure no organic residue remains that might shield microorganisms during sterilisation.
Step Four: Rinsing and Drying
Once the ultrasonic cycle is complete, instruments are rinsed with deionised or distilled water to remove detergent residues. Tap water is avoided because it may leave mineral deposits that cause staining or rusting.
Thorough drying follows rinsing. Moisture trapped inside hinges or lumens can compromise sterilisation, as steam cannot penetrate effectively through water. Facilities typically use medical-grade dryers or compressed air for complete dryness.
Drying is one of the most critical preparatory steps before how to sterilise surgical instruments is carried out.
Step Five: Disinfection and Sterilisation
After cleaning, instruments undergo disinfection or sterilisation, depending on their intended use.
Disinfection involves using chemical agents such as glutaraldehyde or hydrogen peroxide solutions. It eliminates most microorganisms but may not destroy bacterial spores. Disinfection is typically applied to instruments used on intact skin or for non-invasive procedures.
Sterilisation, on the other hand, eradicates all forms of microbial life. It is essential for surgical tools that come into contact with sterile tissues or the bloodstream. Common sterilisation methods include:
1. Steam Sterilisation (Autoclaving)
Autoclaving uses high-pressure saturated steam at temperatures of 121°C to 134°C for a specific duration. It is one of the most reliable and widely used techniques in hospitals and dental clinics. Instruments are placed in autoclave pouches or trays before sterilisation.
2. Dry Heat Sterilisation
Dry heat uses hot air at around 160°C to 180°C to sterilise instruments. It is suitable for tools that might corrode or dull under moist heat, such as certain cutting instruments.
3. Chemical Sterilisation
Chemical sterilants such as ethylene oxide gas or hydrogen peroxide vapour are used for heat-sensitive equipment. These methods require controlled environments and proper aeration to remove toxic residues.
Each of these techniques follows strict guidelines to maintain consistent sterilisation standards across healthcare facilities. For those looking to maintain their own practice, investing in high-quality surgical dental instruments and proper sterilisation systems is essential. You can also get sterile dental equipment in Australia from Dentify Dental today!
Step Six: Inspection and Maintenance
Once sterilised, every instrument undergoes inspection before packaging or storage. Staff check for cleanliness, corrosion, cracks, and proper function. Hinged tools are lubricated using medical-grade lubricants that withstand high temperatures without affecting sterilisation.
Instruments that show damage are repaired or replaced immediately. Regular inspection prevents malfunctions during surgery and maintains patient safety.
Proper labelling and tracking systems are also implemented to record sterilisation cycles, with compliance with healthcare regulations.
Step Seven: Packaging and Storage
Sterile instruments must be packed in clean, moisture-resistant packaging materials that protect them until use. Pouches are labelled with the sterilisation date, operator name, and batch number.
Storage areas are designed to be dust-free and temperature-controlled. Instruments are organised based on procedure type for quick retrieval during surgery.
Proper storage extends the sterility of instruments, reducing the risk of contamination before use.
Bottom Line
The cleaning and disinfection of surgical instruments form the backbone of any safe medical or dental procedure. Each step plays a vital role in protecting patients and healthcare professionals. Clinics that follow strict sterilisation procedures not only protect their patients but also demonstrate professionalism and compliance with dental care standards.
We provide durable, precision-engineered instruments designed for longevity and easy maintenance. Visit our platform to buy dental tools online that meet the highest global sterilisation standards!
Disclaimer
The content provided here on the sterilization, cleaning, and reprocessing of surgical and medical instruments is strictly for informational and educational purposes only. This information is not a substitute for professional training, certification, or the manufacturer's official Instructions for Use (IFU). Sterilization is a critical, complex process that demands strict adherence to regulatory standards; improper technique can cause serious harm, including patient infection. All healthcare personnel must follow their facility's established protocols and the specific IFU for every instrument and piece of equipment. By using this blog, you agree that the author/owner holds no liability for any damages or consequences resulting from the application or misuse of this information.










